If you are over 50 and suddenly finding it hard to sleep through the night, you are not alone. Insomnia is one of the most common symptoms of menopause, affecting up to 61 percent of women in this stage of life.
What was once a natural part of your daily rhythm may now feel like a nightly battle, falling asleep takes longer, staying asleep feels impossible, and waking up too early becomes the norm.
The main culprit is hormonal change. Estrogen and progesterone are the two hormones that play an important role in sleep, they begin to decline in perimenopause and continue to drop after menopause.
Estrogen helps regulate serotonin and melatonin, while progesterone has a natural calming effect on the brain. When levels of these hormones fall, the brain’s ability to stay in deep sleep is disrupted, leaving many women restless at night.
The Link Between Hot Flashes, Night Sweats, and Insomnia
Hot flashes and night sweats are more than just uncomfortable, they are one of the biggest reasons women lose sleep in menopause. When estrogen levels decline, the hypothalamus (the brain’s thermostat) becomes oversensitive, causing the body to overreact to small temperature changes.
This is why you might suddenly wake up drenched in sweat or throw off the blankets in frustration. Research shows that women with frequent hot flashes are far more likely to experience insomnia. The disruption goes beyond the flash itself. Even after the heat passes, it can take time for the body to cool down and settle back into sleep.
Repeated awakenings throughout the night prevent you from reaching restorative deep sleep and can leave you feeling unrefreshed in the morning. This cycle often continues night after night, creating a pattern of chronic sleep deprivation that impacts both physical and mental health.
READ ALSO: Hot Flashes Over 50? What To Do Next…
How Poor Sleep Affects Women Over 50
Sleep is a critical function for memory, mood, and long-term health. During menopause, when sleep is disrupted, women often notice increased irritability, anxiety, or brain fog.
Studies also show that poor sleep raises the risk of depression and worsens other menopause symptoms, creating a frustrating loop where insomnia makes everything else feel worse.
On a physical level, chronic sleep deprivation is linked to weight gain, heart disease, and diabetes. Research suggests that even partial sleep loss can affect metabolism and appetite regulation, which is especially challenging for women already managing midlife changes in body composition.
This makes improving sleep not only about feeling better in the short term but also about protecting long-term health.
READ ALSO: The Surprising Link Between Sleep and Brain Health for Women Over 50: Tips and Insights
Cooling Your Sleep Environment

One of the simplest and most effective ways to reduce menopause sleep problems is to cool your bedroom. Research shows that lowering room temperature can significantly improve sleep quality for women struggling with night sweats.
Using breathable cotton sheets, lightweight sleepwear, and a fan or cooling pillow helps regulate body temperature throughout the night.
The benefit of a cooler environment is not just physical comfort. When your body stays at a stable temperature, the nervous system is less likely to trigger wakefulness. This allows the brain to remain in deeper stages of sleep, which are essential for memory and physical restoration.
Creating a cool sleep environment is a simple lifestyle change that has an immediate effect for many women.
READ ALSO: What to Do When You Can’t Sleep: Practical, Science-Backed Tips for Deep Rest
Building a Consistent Sleep Routine
Routine is one of the most powerful tools for improving sleep during menopause. Going to bed and waking up at the same time every day helps regulate the circadian rhythm, the body’s internal clock that governs sleep and wake cycles.
Research shows that irregular sleep schedules are linked to insomnia and poorer overall sleep quality.
A bedtime routine is equally important. Gentle habits such as reading, stretching, or meditation signal to the brain that it is time to wind down.
Over time, this predictability helps reduce nighttime anxiety and allows the body to shift more easily into rest. For women struggling with frequent awakenings, a consistent routine can be a powerful way to retrain the body toward deeper, more restorative sleep.
The Role of Exercise in Better Sleep

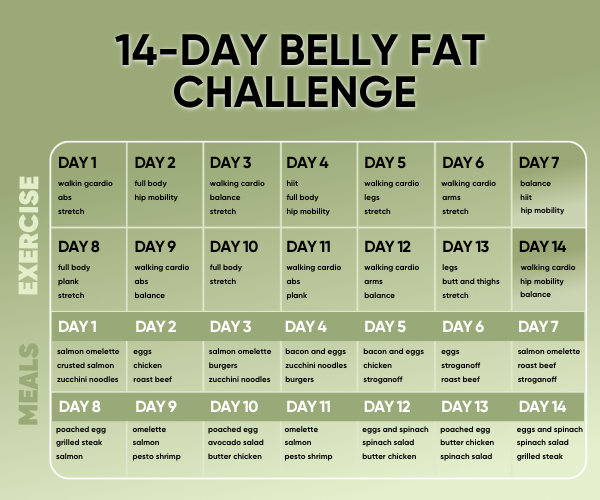
Daily movement is one of the most effective natural remedies for menopause insomnia. Exercise helps regulate mood, lowers stress hormones, and improves overall sleep quality.
A study from the North American Menopause Society found that physically active women reported fewer nighttime awakenings and better sleep compared with sedentary women.
The type of exercise matters less than the consistency. Walking, yoga, swimming, or strength training can all improve sleep. It’s best to exercise earlier in the day, since late-night workouts may leave the body too energized to fall asleep easily.
Beyond sleep, regular movement also reduces hot flashes, strengthens bones, and supports cardiovascular health, making it one of the most important habits for women over 50.
Nutrition and Hydration for Restful Sleep
What you eat and drink has a direct impact on how well you sleep. Caffeine can stay in the bloodstream for up to 10 hours, so avoiding it in the afternoon and evening is essential. Alcohol, while it may make you feel sleepy at first, often disrupts the deeper stages of sleep, leading to more awakenings during the night.
A balanced diet rich in whole foods helps stabilize blood sugar, which prevents middle-of-the-night wake-ups caused by glucose fluctuations. Foods high in magnesium, like leafy greens, nuts, and seeds, support muscle relaxation and melatonin production.
Studies suggest that magnesium intake is associated with better sleep quality. Hydration also matters, but drinking large amounts right before bed can increase trips to the bathroom, so it’s best to hydrate steadily throughout the day.
Stress Reduction and Relaxation Practices

Menopause often brings higher stress and anxiety, both of which fuel insomnia. Stress hormones like cortisol make it harder to fall asleep and can cause the body to wake up too early.
Relaxation practices such as meditation, mindfulness, or deep breathing lower cortisol levels and calm the nervous system, creating the conditions for better rest. Research shows that mindfulness-based stress reduction improves sleep and reduces the severity of hot flashes in menopausal women.
Even short relaxation sessions before bed can make a difference. Ten minutes of slow, mindful breathing or gentle yoga stretches help signal to the body that it is safe to rest.
Over time, these practices not only improve sleep but also reduce anxiety and emotional overwhelm, making daily life feel calmer and more manageable.
Cognitive Behavioral Therapy for Insomnia
Cognitive Behavioral Therapy for Insomnia (CBT-I) is one of the most effective non-drug treatments for sleep problems in menopause. It works by identifying and changing negative thoughts and habits around sleep, helping women break the cycle of anxiety and wakefulness.
Research consistently shows that CBT-I improves sleep quality and reduces insomnia severity in menopausal women.
Unlike sleeping pills, which often provide only short-term relief, CBT-I has lasting effects. Women who complete CBT-I often continue to sleep better long after the program ends because they have learned practical skills to manage sleep disruptions. This approach is particularly useful for women who want a safe, effective, and sustainable solution to insomnia without relying on medication.
When to Seek Professional Support
While natural remedies and lifestyle changes can be very effective, some women continue to struggle with severe insomnia during menopause. In these cases, talking to a healthcare provider is important.
Doctors can help determine whether other conditions, such as sleep apnea or thyroid issues, are contributing to sleep problems. They can also discuss whether hormone replacement therapy (HRT) or non-hormonal medications might be helpful.
HRT is the most effective treatment for hot flashes and night sweats, and by reducing these symptoms, it often improves sleep. However, it is not suitable for everyone, and the risks and benefits should be carefully discussed with a healthcare professional.
Seeking medical advice ensures that you are not overlooking any underlying health concerns and gives you access to a full range of treatment options.
Final Thoughts
Sleep problems in menopause are common, but they are not inevitable. By understanding how hormonal changes affect sleep and making adjustments in lifestyle, environment, and mindset, women over 50 can dramatically improve their rest.
Cooling the bedroom, sticking to a routine, exercising regularly, and practicing relaxation techniques are powerful steps that can bring immediate relief.
Restful sleep is essential for physical health, emotional balance, and overall vitality. While the menopause transition can be challenging, it is also a time to embrace new habits that support long-term wellness.
With patience, persistence, and the right strategies, better nights and brighter days are entirely within reach.
FAQs: How to Sleep Better During Menopause
Your estrogen and progesterone levels are dropping, and both hormones play a direct role in regulating sleep. Without them, your body temperature swings, your stress hormone spikes overnight, and your sleep becomes lighter and easier to disrupt.
This is often a cortisol issue. As estrogen declines, cortisol, your stress hormone, tends to surge earlier in the night than it should, jolting you awake in the early hours, sometimes with a racing heart or anxious thoughts.
They’re a big one, but not the only one. Night sweats fragment your sleep, but menopause also changes your sleep architecture overall, meaning you spend less time in deep, restorative sleep even on nights without obvious sweating.
It can help if your issue is falling asleep, but it won’t fix night sweats or early morning waking. It’s a mild sleep aid, not a solution to the underlying hormonal disruption driving most menopause sleep problems.
Drop your bedroom temperature to between 65 and 68°F, skip alcohol with dinner, and keep your phone out of the bedroom. None of these fix the root cause, but they remove common triggers that make menopause sleep problems worse, and you’ll likely feel the difference by morning.