What exactly are the 3 stages of menopause and where are you in all of this?
If you’re in your 40s or 50s and wondering, “Is this perimenopause? Menopause? Am I through it yet?” you are not alone. Many women reach midlife feeling confused because nobody really explained how this transition works, especially the three stages:
- Perimenopause (the hormonal rollercoaster)
- Menopause (the one-year marker)
- Postmenopause (everything after that)
Let’s walk through the three stages of menopause and what you can do when your periods are irregular and you’re sweating through the sheets.
Key Takeaways: What Are The 3 Stages of Menopause
- Perimenopause is the lead-up phase. Your hormones start to swing, your periods change, and symptoms like hot flashes, mood changes, and poor sleep often begin, even though you’re still having periods.
- Menopause is reached when you’ve had 12 months in a row with no period (and there’s no other clear reason like pregnancy or illness). It’s technically one point in time, not a long phase.
- Postmenopause is everything after that 12-month mark. Your hormones settle at a new, lower level. Some symptoms ease, and long-term health topics like bones, heart health, and weight become more important.
- If your cycles are changing and you don’t feel like yourself, you’re likely somewhere on this path and there is help and support at every stage.
What are the 3 stages of menopause?
Menopause is a transition, it’s not something that happens in a single day.
- Perimenopause refers to the period leading up to menopause, during which your hormones begin to fluctuate and symptoms start to appear, despite the fact that your periods are still occurring.
- Menopause is the natural biological stage in a woman’s life that signifies the permanent end of menstruation and reproductive ability. It’s officially diagnosed after 12 consecutive months without a period.
- Postmenopause refers to the period of time following the 12-month mark. Your hormones settle into their new, lower levels, and some symptoms improve while others (like bone and heart health changes) need more attention.
So when you say, “I’m in menopause,” you’re often talking about the whole journey, but medically, there’s a bit more nuance.
How do I know if I’m in perimenopause?

This is one of the most common questions midlife women ask.
Perimenopause usually starts in your 40s, but for some women it begins earlier or later. It can last anywhere from a couple of years to 7–10 years for some.
Here are some typical signs that you might be in perimenopause:
- Your periods may be closer together, farther apart, lighter, heavier, or just not follow a pattern.
- You start noticing hot flushes or night sweats, especially before your period.
- Your sleep gets worse, even when you feel tired.
- Mood seems more fragile, with irritability, anxiety, a low mood, and brain fog.
- PMS feels more intense or lasts longer than it used to.
- You notice weight creeping on, especially around the tummy, even if your habits haven’t changed much.
You might still be having regular periods and think, “It can’t be menopause yet.” But perimenopause is all about hormone fluctuations, not just the final period. Your estrogen and progesterone are going up and down more dramatically, and your brain and body feel those swings.
READ ALSO: What Is Perimenopause? Symptoms, Bloating, Diet and Weight Changes Explained
How is menopause different from perimenopause?
Many women use “menopause” to cover everything, but medically:
- Perimenopause = irregular hormone swings + changing cycles + emerging symptoms.
- Menopause = the moment you’ve gone 12 months in a row without a period (without pregnancy, illness, or other medical reasons).
If you have not had a period for 8 or 9 months and then experience a random period, you are still in perimenopause. The clock resets, and you’ll need another 12 period-free months to reach official menopause.
Menopause is therefore a date on the timeline rather than a protracted stage. You tend to feel the most about everything around it, both before and after.
What is postmenopause and what changes after that 12-month mark?
Postmenopause starts the day after your “menopause anniversary,” meaning you’ve gone one full year without a period.
In postmenopause:
- Your estrogen and progesterone are at their new, lower baseline instead of swinging wildly like in perimenopause.
- Some symptoms, like wildly unpredictable cycles and very intense PMS often calm down.
- Hot flashes and night sweats may get milder or less frequent over time for many women, though some continue to have them for years.
- Longer-term questions become more important: bone health, heart health, muscle strength, brain health, weight management, and sleep quality.
The day your periods stop, you’re not “past it all”. Your body has entered a new hormonal state that will last for the rest of your life. That’s why changes to your lifestyle and sometimes hormone replacement therapy (HRT) can still be important after your periods are over.
How long does each stage of menopause usually last?

There’s no exact schedule, which is why it can feel so confusing.
Rough guides (these are averages, not rules):
- Perimenopause: around 2–7 years for many women, sometimes longer.
- Menopause: when you hit 12 months without a period.
- Postmenopause: from that point on.
You might hear women say, “I was in menopause for 10 years.” Usually, they are referring to the entire transition period, particularly perimenopause and the early years of postmenopause when symptoms were most severe.
Everyone’s story is different, and that’s normal.
What symptoms are most common in perimenopause?
Perimenopause is often the messiest, most confusing stage because you’re still cycling – but your hormones are less predictable.
Common perimenopause symptoms include:
- Cycle changes: shorter, longer, heavier, lighter or skipping months.
- Hot flushes and night sweats often begin around the time of your period.
- Sleep problems: difficulty falling asleep or waking up at 3 a.m. with a racing mind.
- Mood changes: anxiety, irritability, low mood, sudden crying spells.
- Brain fog and poor concentration.
- Breast tenderness and bloating before periods that feels different to your old PMS.
- Headaches or migraines around your period.
- Vaginal dryness or discomfort, and lower libido.
- Weight gain around the middle, feeling “puffy” or inflamed.
You don’t need to have all of these in perimenopause. Even two or three of them, alongside changing cycles, can be a sign.
Should I get a hormone test to see if I’m in perimenopause?

For most women in their 40s and early 50s, a doctor can make a clinical diagnosis of perimenopause based on:
- Your age
- Your changing periods
- Your symptom pattern
Hormone tests (like FSH, LH, and estrogen) can be up and down from week to week, so a blood test isn’t always reliable. A “normal” result does not mean your symptoms aren’t real.
When hormone tests may be useful:
- You’re having symptoms very early (for example, in your 30s).
- Your periods have stopped suddenly, and your doctor wants you checked for premature ovarian insufficiency or other conditions.
- You’re using hormonal contraception that masks your natural cycle (like some IUDs or pills) and it’s harder to tell what’s going on.
But in many cases, your story and symptom pattern is enough for a doctor who understands menopause well.
What actually happens to my hormones in each stage?
In perimenopause
- Estrogen goes up and down more sharply, and not just “down.”
- Progesterone often falls earlier and faster because you might not ovulate every cycle.
- This combination can mean stronger mood swings, heavier or unpredictable bleeding, and more sleep issues.
In menopause / early postmenopause
- In the end, estrogen and progesterone levels both drop.
- As the ovaries become less responsive, your brain sends more signals to them through hormones like FSH and LH.
- The big mood swings get better, but you still have less oestrogen in your body.
That lower estrogen affects:
- Bones (more risk of bone loss over time)
- Skin (thinner, drier, more wrinkles)
- Vaginal tissue (more dryness and discomfort)
- Heart and blood vessels
- Brain chemistry (mood, sleep, and memory pathways)
This is why many women focus on strength training, protein, bone health, and cardiovascular health after 50.
READ ALSO: Tips to Help You Balance Menopause and Mental Health
Is postmenopause “better” than perimenopause?

Yes, for some women, because their hormones stop going crazy.
Many women say:
- Their mood feels more stable.
- PMS-type symptoms ease.
- They feel a new sense of clarity and they say, “this is who I am now.”
But there can be new challenges:
- Ongoing hot flashes or night sweats for some.
- Vaginal dryness, discomfort with sex, or recurrent UTIs.
- Noticeable changes in skin, hair, joints and weight.
- More focus is needed on bones, heart, blood pressure, and cholesterol.
So it’s not about “better or worse,” but what your body needs now and how to support it.
Can you still get pregnant in each stage?
This is a practical worry for many.
- Perimenopause: Yes, you can still get pregnant. Ovulation becomes less predictable, not impossible. If you don’t want pregnancy, you still need contraception until you reach menopause.
- Menopause: Once you’ve reached 12 months with no period (and you’re over 50), natural pregnancy is extremely unlikely.
- Postmenopause: Pregnancy is not expected. If you ever have new vaginal bleeding after menopause, it’s a reason to see a doctor, not a sign of fertility returning.
If you’re under 50, some guidelines suggest waiting 2 years without a period before you stop contraception. It’s worth checking local guidance and talking to your doctor.
What symptoms are “normal” and when should I worry?
Menopause symptoms can be uncomfortable, but some “red flags” need a doctor’s attention.
Common but usually not dangerous:
- Hot flashes and night sweats
- Irregular periods in your 40s / early 50s
- Mood swings, brain fog, sleep problems
- Vaginal dryness or discomfort
- Weight gain, joint aches, mild headaches
See a doctor promptly if:
- You have very heavy bleeding, bleeding between periods, or bleeding that continues for a long time.
- You are bleeding after 12 months with no period (postmenopausal bleeding).
- You have chest pain, sudden shortness of breath, or symptoms that feel like a heart attack or stroke.
- Your mood is very low, you feel hopeless, or you have thoughts of harming yourself.
- You wake up gasping or snore very loudly and feel exhausted (possible sleep apnoea).
Your symptoms are real. You don’t need to wait and see if something feels “off” or scary; your doctor is there to help.
How do I know if I’m “through” menopause?

You are technically “through” menopause when you’re in postmenopause, meaning more than 12 months since your last period. But many women still get symptoms well into their 50s and sometimes 60s, especially hot flashes, sleep issues and joint pain.
So instead of waiting to be “done,” it can be helpful to ask:
- What stage am I in now (peri, around the 12-month mark, or postmenopause)?
- What are my biggest symptoms right now?
- What support (lifestyle changes, HRT, other treatments) could help this stage?
You can feel better within each stage. You don’t have to wait for it to be over to get your life back.
Should I consider HRT or try to manage naturally?
There’s no one right answer; it depends on:
- Your symptoms
- Your medical history
- Your personal preferences and risk factors
Hormone Replacement Therapy (HRT) can:
- Reduce hot flashes and night sweats
- Improve sleep, mood and quality of life for many women
- Help protect bone density and, for some women starting at the right age/time, may support heart health
Some women prefer to start with lifestyle changes, supplements, and non-hormonal options. Others choose HRT early because their symptoms are affecting work, relationships, or mental health.
What matters most is informed choice:
- Talk to a doctor or menopause specialist you trust.
- Discuss your risks (family history, personal history, age, timing since last period).
- Review both hormonal and non-hormonal options.
Choosing HRT doesn’t mean you’re “weak”, and not choosing it doesn’t mean you’re “braver”. It’s simply about what helps you live well.
READ ALSO: How Long Does It Take For Hormone Replacement Therapy To Work Effectively?
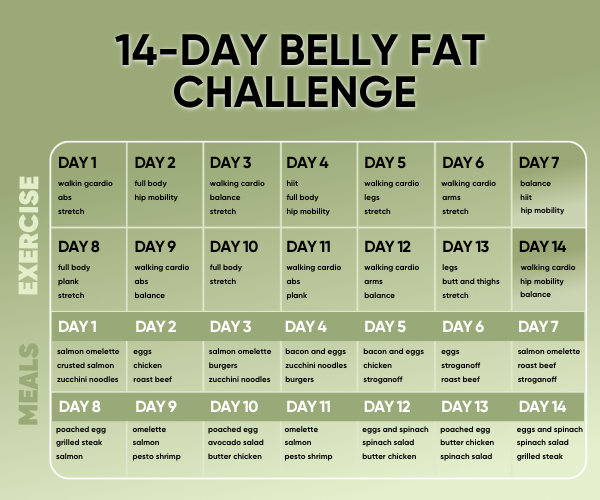
What can I do in each stage to feel better and stay healthy?

Here’s a simple way to think about it:
In perimenopause
Focus on:
- Sleep routines and calming evening habits
- Regular movement, especially strength training 2–3 times a week
- Balanced meals with protein, healthy fats, fibre (to help blood sugar and mood)
- Stress support: breathing exercises, yoga, therapy, journaling
- Talking with your doctor early if symptoms are affecting your daily life
Around menopause / early postmenopause
Focus on:
- Exploring HRT or other treatments if symptoms are strong
- Bone health: calcium, vitamin D, strength training, walking
- Heart health: blood pressure, cholesterol, regular check-ups
- Vaginal comfort: moisturisers, lubricants, or local estrogen if recommended
In postmenopause
Focus on:
- Keeping muscle and strength (this protects joints, bones, and metabolism)
- Keeping your mind and body active by staying socially and mentally active
- Regular health checks (breasts, blood pressure, and bone scans if needed)
- Treating vaginal, bladder, or sexual discomfort, you don’t just have to live with it
Don’t just get through the symptoms; think of each stage as a chance to help your future self.
Closing thoughts
If you’ve ever felt lost or confused during the three stages of menopause, you’re not broken. You’re going through a change that most women aren’t ready for.
You can ask, “Where am I on this journey?” You can say, “I need better care, better sleep, and better information.” You can be hopeful about the woman you’re becoming on the other side.
Perimenopause, menopause, and postmenopause are not three doors that close. They’re parts. You get to decide how this chapter looks and feels, with knowledge, support, and a lot more kindness towards yourself than you were ever taught to give.
FAQs: The 3 Stages of Menopause
If you’re in your 40s or early 50s and your periods have changed (shorter, longer, heavier, lighter, skipping months) plus you’re noticing symptoms like hot flashes, night sweats, mood swings, brain fog or new sleep problems, you’re very likely in perimenopause. A doctor can usually confirm this just from your age, cycle pattern, and symptoms.
Yes. Ovulation becomes less reliable but doesn’t stop straight away. Pregnancy is still possible until you reach menopause, so you still need contraception if you don’t want to get pregnant.
Menopause is officially the point when you’ve had 12 months in a row with no period and there’s no other obvious cause. If you go 7–8 months without a period and then bleed again, you’re still in perimenopause and the 12-month countdown resets.
Postmenopause starts the day after your “12 months with no period” mark. Hormones are lower but more stable, rather than swinging up and down as they do in perimenopause. Unpredictable cycles and crazy PMS tend to settle, but you may still have hot flashes, sleep issues, vaginal dryness, and longer-term changes in bones, heart health, and metabolism to look after.
There’s no fixed schedule. Perimenopause often lasts a few years and sometimes up to seven or more. Menopause itself is a single time point (the 12-month mark). Postmenopause then continues for the rest of your life. Symptom intensity can rise and fall within these stages rather than following a perfect line.
Not always. Hormone levels can move around a lot in perimenopause, so one blood test can be misleading. For most women in their 40s and 50s, doctors look first at age, period pattern, and symptoms. Blood tests are more useful if you’re younger, have very unusual symptoms, or your doctor wants to rule out other conditions.
Yes, it can be. Many women continue to have hot flashes, sleep problems, joint aches, or vaginal symptoms into postmenopause. It’s common, but that doesn’t mean you have to put up with it. Lifestyle changes, local treatments, HRT, and non-hormonal medicines can all be options to discuss with a doctor.
Irregular bleeding is common in perimenopause. Still, see your doctor if your bleeding is very heavy, lasts a long time, or happens between periods. Any bleeding that happens after 12 months with no period (postmenopausal bleeding) should always be checked promptly, as it can sometimes be a sign of something more serious.
No. Some women feel well with lifestyle changes, stress support, and local treatments alone. Others find their quality of life improves a lot with HRT. The “right” choice depends on your symptoms, medical history, risks, and personal preferences. What matters is that you’re given clear information and options, not left to suffer.
In perimenopause, focus on calming the swings: better sleep habits, regular movement, stress support, and a nutrient-dense diet. Around menopause and early postmenopause, bone, heart, and muscle health need more attention, and this is when many women consider HRT. In postmenopause, keep lifting weights, stay active, nourish your body well, keep up with health checks, and seek help for ongoing symptoms rather than silently coping.