Most women spend years worrying about breast cancer. Far fewer know that heart disease is the leading cause of death in women over 50, responsible for more female lives lost than all cancers combined. And most don’t know that menopause is one of the most significant moments in a woman’s cardiovascular life, a transition point where risk doesn’t just inch upward but shifts in ways that demand attention.
Menopause is also the season when your long-term heart risk starts to rise, mainly because estrogen changes can affect cholesterol, blood vessels, blood pressure, sleep, stress, and where your body stores fat.
This guide helps you understand what changes in menopause that affects the heart, which symptoms are common, and when it’s time to take symptoms seriously and get checked.
Key Takeaways
- Menopause doesn’t “doom” your heart, but it can shift key risk factors (cholesterol patterns, blood pressure trends, belly fat, inflammation, sleep).
- Hot flashes can include heart pounding, but chest pain, shortness of breath, fainting, or new severe symptoms should never be brushed off.
- Your most powerful protection after 50 is boring (and effective): daily movement, strength training, heart-supportive eating, sleep and stress regulation.
- The best “first step” is a simple check-in: blood pressure, lipids, blood sugar, waist changes, and family history, then build your plan from there. (This is the reset window.)
- If you’re ever unsure whether it’s a hot flash or something urgent, err on the side of safety and get assessed.
Worried About Your Heart in Menopause? Start Here
If you’re reading this and thinking, “This sounds like me… but I’m not sure what I’m feeling,” you’re in the right place.
Menopause can create sensations that mimic heart symptoms, and because women’s symptoms don’t always look the same as men’s, it can feel even more confusing. Some women notice palpitations during hot flashes. Others notice a tightness in the chest after poor sleep, stress, caffeine, or anxiety. And sometimes it’s simply a body reacting to hormonal shifts.
Are your symptoms mostly coming in waves (and passing), or are they new, strong, and getting worse?
- If the symptoms come in waves, such as heat rising, sweating, heart pounding, and then easing, it may be related to hot flashes, stress, or nervous system shifts in menopause.
- If the symptoms are new, persistent, or feel frightening, especially chest pressure, faintness, nausea, or shortness of breath, treat it as urgent and get checked.
From there, use the links below based on what you’re trying to figure out right now.
Start here
These are the two cluster posts that live under this sub-pillar:
- Menopause and Heart Disease: What Changes After 50 and How to Protect Your Heart
- Hot Flashes or Heart Attack? How to Tell the Difference and Know When to Get Help
Want the full overview first? Start here: Menopause Over 50 (Complete Guide)
Why Menopause Changes Your Heart Risk

For most of your adult life, estrogen worked quietly in your favor. It helped keep your arteries flexible and responsive, supported healthy cholesterol levels by keeping LDL low and HDL high, reduced inflammation in blood vessel walls, and helped regulate blood pressure. It was, in many ways, a built-in cardiovascular protector.
When estrogen declines during perimenopause and menopause, that protection fades. And the changes that follow aren’t gradual. Research shows that within the first few years after menopause, LDL cholesterol rises significantly, HDL cholesterol drops, triglycerides increase, and arterial stiffness begins to develop more rapidly. Blood pressure that was perfectly controlled in your 40s can become harder to manage in your 50s without any change in lifestyle.
At the same time, the fat redistribution that comes with menopause, moving from the hips and thighs toward the abdomen, adds another layer of risk. Visceral fat, the kind that accumulates around your organs, is metabolically active in ways that drive inflammation, insulin resistance, and elevated cardiovascular risk. It is not just an aesthetic change. It is a health signal.
The Symptoms Women Miss
Heart attack symptoms in women often look different from the classic Hollywood version of a man clutching his chest. Women more commonly experience fatigue that feels different from normal tiredness, shortness of breath, nausea, jaw or neck pain, upper back discomfort, and a vague sense that something is wrong. These symptoms are easier to dismiss and are frequently attributed to menopause, anxiety, or simply getting older.
This is a dangerous gap. Women are statistically more likely to delay seeking care during a cardiac event, and they are more likely to be misdiagnosed or undertreated when they do. Knowing your personal risk and knowing the full range of symptoms are not optional. They are potentially life-saving pieces of information.
Hot flashes also deserve more attention in this conversation than they typically receive. Research now links frequent, severe vasomotor symptoms to a higher risk of cardiovascular events. Women who experience intense hot flashes, particularly those that persist for many years, show greater rates of arterial stiffness and endothelial dysfunction than women with milder symptoms. The hot flash is not just a nuisance. It may be a window into what is happening in your vascular system.
The Numbers You Need To Know
You cannot manage what you do not measure. There are five numbers every woman over 50 should know and understand.
Your blood pressure should be below 120 over 80. Readings that creep into the 130s are worth a conversation with your doctor, even if they fall into what is still technically a “normal” range.
Your LDL cholesterol should ideally be below 100 milligrams per deciliter, and your HDL should be above 50. Triglycerides below 150 are the target.
Your fasting blood sugar should be below 100, and your body mass index, while an imperfect measure, is still a useful screening tool when combined with waist circumference, which should be below 35 inches for women.
If you don’t know these numbers, get them. Your annual physical is the right time to ask for a full lipid panel, blood pressure check, and fasting glucose. If your doctor isn’t reviewing these with you in the context of menopause, it is worth raising directly.
Know your numbers, know your body. Calculate your BMI and BMR today and take the guesswork out of your health journey.
What Actually Protects Your Heart After 50

Move consistently, and include strength training
Cardiovascular exercise is the most studied and most effective lifestyle intervention for heart health. But after 50, adding resistance training matters too.
Strength training improves insulin sensitivity, reduces visceral fat, lowers blood pressure, and supports the vascular health that cardio alone doesn’t fully address. You don’t need to train like an athlete. You need to be consistent, most days of the week, with a mix of both.
Helpful next read: What Is the Complete Menopause Timeline From First Signs to Long-Term Health?
Eat for your cardiovascular system specifically
The Mediterranean diet has the strongest evidence base for cardiovascular protection in menopausal women. This means olive oil as your primary fat, fatty fish two or more times per week, abundant vegetables and legumes, whole grains, nuts, and seeds, with red meat and ultra-processed foods kept to a minimum.
It also means significantly reducing sodium, which becomes more impactful on blood pressure after estrogen withdrawal. This is not a diet in the punishing sense. It is a way of eating that happens to be both delicious and deeply protective.
Read next: What Really Happens to My Estrogen and Hormones During Menopause?
Don’t dismiss stress and sleep as secondary
Chronic stress raises cortisol, which raises blood pressure, promotes inflammation, and accelerates arterial damage. Poor sleep does the same.
Women who are sleeping badly during menopause are not just tired. They are running with elevated cardiovascular risk every single day. Treating sleep disruption and managing stress are not soft recommendations. They are hard cardiovascular ones.
Explore postmenopause here: What Does Life Look Like in Postmenopause After Your Periods End?
Talk to your doctor about hormone therapy
The conversation around HRT and heart health is more nuanced than the fear-based narrative many women absorbed in the early 2000s.
Current evidence suggests that for healthy women under 60, or within 10 years of menopause onset, hormone therapy does not increase cardiovascular risk and may in fact be protective when started early in the transition.
Timing matters significantly here, and the conversation is worth having with a menopause-informed provider who can assess your individual risk profile.
Explore postmenopause here: What Does Life Look Like in Postmenopause After Your Periods End?
Know your family history and act on it
If heart disease runs in your family, menopause is the moment to take that seriously. Genetic risk becomes more relevant when your hormonal protection diminishes.
A calcium scoring scan, which measures plaque buildup in your coronary arteries, is a low-cost, low-radiation tool that can give you a clearer picture of your actual cardiovascular risk beyond what standard bloodwork shows.
Explore postmenopause here: What Does Life Look Like in Postmenopause After Your Periods End?
The safety rule: when to get help
This is the simplest way to think about it:
If symptoms feel new, intense, unusual for you, or scary, don’t argue with yourself. Get checked.
You can still learn menopause patterns and take your health seriously at the same time. Both can be true.
What protects the heart during menopause
The heart-protective basics are simple, but powerful:
- regular walking or gentle cardio you can sustain
- strength training to support metabolism and reduce visceral fat
- a heart-supportive eating pattern (Mediterranean-style is a great foundation)
- sleep support and stress regulation
- keeping track of your numbers (BP, cholesterol, blood sugar)
- treating symptoms early instead of waiting until they become chronic
The Takeaway
Heart disease is not a men’s health issue. It is the leading threat to women’s lives after 50, and menopause accelerates the timeline in ways most women are never told about clearly enough.
You have more control over this than you might think. The right numbers, the right habits, the right conversations with your doctor, and the right timing all make a real difference. Your heart has been working for you your entire life. After 50, it needs you to start working for it.
Related Resources: Heart Health and Menopause
- Essential Guide to Heart Health for Women: Risks and Prevention
- The Complete Menopause Timeline From the First Signs
- Menopause Symptoms by Stage: The Timeline Explained
- Why Strength Training Is Essential During Menopause & After 50
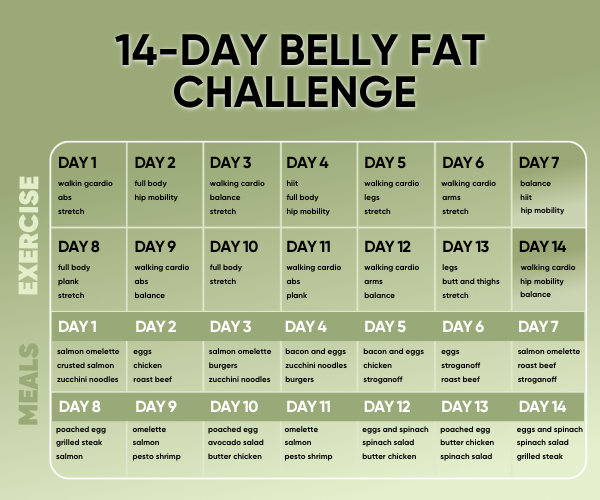
- Menopause Meal Plans That Work for Women Over 50
- Zone 2 Walking for Longevity: A Beginner’s Guide
- How to Sleep Better During Menopause
- Is It a Hot Flash or a Heart Attack? How to Tell the Difference and Stay Safe
- How Does Menopause Affect Heart Disease Risk? Key Facts for Women Over 50
FAQs: Heart Health and Menopause
Yes. Many women notice palpitations during hot flashes, poor sleep, stress spikes, dehydration, or caffeine. It can feel intense, but it’s often linked to hormonal and nervous system shifts.
Look at the pattern. Hot flashes tend to come in waves and pass. Symptoms that are new, severe, persistent, or worsening — especially chest pressure, fainting, or shortness of breath, should be treated as urgent.
Because the hormonal shift can affect cholesterol, blood vessels, inflammation, metabolism, and fat storage patterns over time. It’s not immediate danger, it’s long-term risk that’s worth managing.
A mix of consistent walking/cardio and strength training. Walking supports cardiovascular health, while strength training supports metabolism and helps reduce visceral fat, a key risk factor.
If you’re having symptoms you don’t understand, yes, and even without symptoms, it’s smart to monitor your baseline numbers after 50 (blood pressure, cholesterol, blood sugar).
Yes. Anxiety can cause chest tightness, breathlessness, and a racing heart, and menopause can make anxiety more common due to sleep disruption and hormone shifts. The feeling is real, even when the cause isn’t dangerous.
Your Next Step
If you’re in the “I just want to feel normal again” season, start with our Complete Menopause Guide for Women Over 50 to understand what’s happening and why. Then grab our Menopause Meal Plans to fuel your body with what it actually needs right now.
Want a simple 7-day menopause reset to feel more like you again? If you’re in the foggy, tired, “what is happening to my body?” season, this is a gentle way to get momentum, without extreme rules. You’ll get a clear daily structure that supports energy, mood, and consistency. Join the 7-Day Menopause Smart Kickstart Challenge
You can also explore our Menopause & Nutrition Weight Loss Bundle for a complete reset. Clarity reduces anxiety and helps you choose the right support for where you are.
Want the full overview first? Start here: Menopause Over 50 (Complete Guide)