If you’ve ever thought, “What on earth is happening to my hormones?” you are not alone. One month you feel mostly yourself, the next you’re hot, wired, teary, awake at 3 a.m., and wondering where your old brain and body went.
Menopause can feel like a mystery that nobody ever properly explained, and it’s easy to blame yourself, your willpower, your attitude, and your mindset. But nothing about what you’re feeling is your fault.
Menopause is a real, biological shift. Your estrogen, progesterone and other hormones are moving through a powerful transition, and your symptoms are your body’s way of saying, “Something big is changing.”
When you understand what actually happens to estrogen and hormones during menopause, you move from confusion to clarity and from feeling like your body is working against you to feeling like you’re working with it.
But what happens to your estrogen during menopause? If you’ve been wondering about this, here’s everything you need to know about menopause and your hormones.
The more you know about menopause and estrogen, the better you can manage your hormones.
Quick Answer: What Happens To Your Hormones in Menopause
- During perimenopause and menopause, your ovaries slowly make less estrogen and progesterone.
- These hormones no longer rise and fall in a smooth monthly cycle, they become chaotic, then gradually fall to a new lower “baseline.”
- This shift affects periods, sleep, mood, hot flashes, weight, joints, brain, and heart health.
- Estrogen levels fluctuate wildly, then drop
- Progesterone usually falls earlier and faster than estrogen
- FSH and LH rise as your brain tries to “push” the ovaries.
- Other hormones such as insulin, cortisol, and thyroid also feel the ripple, affecting weight, belly fat and energy.
- Hormone changes affect temperature control, mood, bones, heart, and metabolism
- You can support your hormones in menopause with lifestyle, medical options (like HRT when appropriate), and targeted self-care.
What Exactly Is Menopause and When Does It Start?
Menopause is officially the point in time when you’ve gone 12 months without a menstrual period that isn’t due to pregnancy or another cause. The average age is around 51–52, though anywhere between about 45 and 55 is considered normal.
Menopause itself is just one day on the timeline. The years around it, when most of the chaos happens, are when the story of hormones really comes to life.
Perimenopause, Menopause and Postmenopause in Simple Terms
- Perimenopause: The “run-up” to menopause. It can start in your 40s and last several years. Periods become irregular, estrogen and progesterone rise and fall like a rollercoaster, and symptoms such as hot flashes, heavy periods, mood swings and sleep issues often begin.
- Menopause: The 12-month mark without a period. Once you pass this, you are said to be in menopause. This means that your ovaries are “retiring” and no longer releasing eggs.
- Postmenopause: All the years after that 12-month mark. Estrogen and progesterone are now consistently lower. Some symptoms may ease, but long-term health areas like bone strength and heart health need extra care because of the lower estrogen.
It’s like a three-act play: it goes up and down, stops, and then settles into a new, more stable phase.
READ ALSO: Everything You Should Know About Perimenopause
The Menopause Hormone Shift: 4 Key Hormones to Know

Let’s look at the main hormone players so you can finally answer: What happens to my estrogen and hormones during menopause?
Estrogen
What estrogen normally does
Estrogen isn’t just a “period hormone.” It helps:
- Regulate your menstrual cycle and fertility
- Maintain bone density and muscle mass
- Support your heart and blood vessels
- Influence brain function, mood and memory
- Keep vaginal tissue, bladder and skin healthy and flexible.
This is why changes in estrogen during menopause can be felt everywhere, from your joints to your emotions.
What happens to your hormones during perimenopause?
During perimenopause, estrogen doesn’t simply “go down.” It spikes high and crashes low, often unpredictably.
That pattern can cause:
- Heavy or erratic periods
- Breast tenderness
- Mood swings and irritability
- Migraines in some women
- Episodes of hot flashes or night sweats
Many women say, “I feel like I’m on a hormonal rollercoaster”and biologically, that’s exactly what’s happening.
What happens to your hormones during menopause/postmenopause?
After menopause, estrogen settles at a much lower, steady level.
Lower estrogen is linked to:
- Increased bone loss and osteoporosis risk.
- Higher risk of heart disease over time.
- Vaginal dryness, discomfort with sex and urinary symptoms.
- Shift in fat storage from hips/thighs toward the abdomen.
So if you’re wondering why “everything changed” around your belly, your bones, your mood and your sleep, that’s the estrogen story.
Progesterone
What progesterone normally does
Progesterone is your body’s “steadying” hormone. It:
- Helps prepare the uterus for pregnancy
- Balances estrogen to keep periods from becoming too heavy
- Has a naturally calming, sleep-supporting effect on the brain
What happens in midlife
Progesterone often drops earlier and more steadily than estrogen in perimenopause.
This can look like:
- Sleep problems, especially trouble staying asleep
- Feeling more anxious or “on edge”
- Heavier or more irregular periods (because estrogen is unopposed)
That early drop in progesterone is a big reason why you might feel like your nervous system lost its “soft blanket.”
FSH and LH
FSH (follicle-stimulating hormone) and LH (luteinizing hormone) are signals from the pituitary gland in your brain to your ovaries.
- In reproductive years, they help trigger ovulation.
- As the ovaries become less responsive with age, the brain turns up the signal, FSH and LH rise.
That’s why:
- A high FSH level (along with symptoms) can be one marker that you’re in the menopausal transition or past it.
- Labs sometimes report results as in the “menopausal range.”
FSH and LH are like your brain telling the ovaries to make more noise until the line goes quiet.
Other Hormones That Feel the Ripple Effect
The estrogen and progesterone shifts don’t happen in isolation. They ripple into other systems:
- Insulin: Lower estrogen can promote insulin resistance and increases in central (belly) fat, which is linked to higher risks of diabetes and metabolic syndrome.
- Cortisol: Chronic stress plus midlife changes can keep cortisol high, promoting belly fat, poor sleep and cravings.
- Thyroid hormones: Thyroid issues are more common in midlife; low thyroid hormones slow metabolism and cause fatigue, weight changes and cold feelings.
So if you feel “off” in more than one area at once, it’s not just estrogen. It’s the whole hormonal network.
READ ALSO: How You Can Find Balance During Menopause Over 50
How Do Hormone Changes Cause My Symptoms?

During menopause, your hormones change, especially estrogen and progesterone, which can cause hot flashes, brain fog, weight gain, anxiety, and poor sleep. These changes affect how your brain, temperature control, sleep, mood, metabolism, and joints work.
How Do Hormone Changes Cause Hot Flashes and Night Sweats?
- Estrogen helps the brain’s temperature control centre keep your body in a comfortable range.
- When oestrogen levels change and then drop, the brain can misread your temperature and think you’re too hot, which causes a “cooling response.” This makes your blood vessels open up, your heart rate speed up, and you sweat a lot. This is how hot flashes and night sweats happen.
Common hot flash triggers:
- Alcohol
- Stress or anxiety
- Spicy foods
- Caffeine
- Overheating at night (heavy bedding, hot room)
If you know the “why,” it’s easier to try new ways of living and, if necessary, talk to your doctor about treatment.
Why Do My Mood and Sleep Change So Much in Menopause?
Mood and sleep are often where women feel the hormone story most deeply.
- Lower progesterone means less of that natural calming, sleep-supporting influence.
- Estrogen changes affect brain chemicals like serotonin and dopamine, which influence mood, anxiety and emotional resilience.
This can show up as:
- 3 a.m. waking with a racing mind
- Irritability or feeling “snappy”
- Low mood or increased anxiety
- Brain fog and difficulty concentrating
You’re not “losing it.” Your brain is responding to real hormonal shifts and it can be supported.
READ ALSO: Signs You Have a Hormonal Imbalance and How To Treat It
Why Do Hormones Affect My Weight, Belly and Energy?
If you’re suddenly gaining weight around your middle despite not changing much, you’re not imagining it.
- Lower estrogen is linked to a shift from lower-body fat (hips/thighs) to more visceral belly fat.
- Muscle mass naturally declines with age, which slows your resting metabolic rate, so you burn fewer calories at rest.
- Insulin and cortisol changes can create more cravings, energy crashes and that “tired but wired” feeling.
This is why “just eat less and exercise more” usually doesn’t work well after 50. Your hormonal landscape has changed, so your strategy needs to change too.
READ ALSO: Why You’re Gaining Weight Even When You Eat Less
How Do Hormones Affect My Bones, Heart and Long-Term Health?
Estrogen is deeply protective over the long term:
- Bones: Estrogen helps maintain bone density; when it falls, bone loss accelerates, raising the risk of osteoporosis and fractures.
- Heart and arteries: Estrogen helps keep blood vessels flexible and affects cholesterol; lower levels are linked with rising cardiovascular disease risk after menopause.
This is why menopause is considered a key window for heart and bone health and why strength training, nutrition and sometimes HRT become important conversations.
READ ALSO: 5 Top Foods to Deal With Menopause Symptoms
What Can I Do to Support My Hormones in Menopause?

You can’t stop menopause, but you can make the ride smoother.
Helpful daily habits:
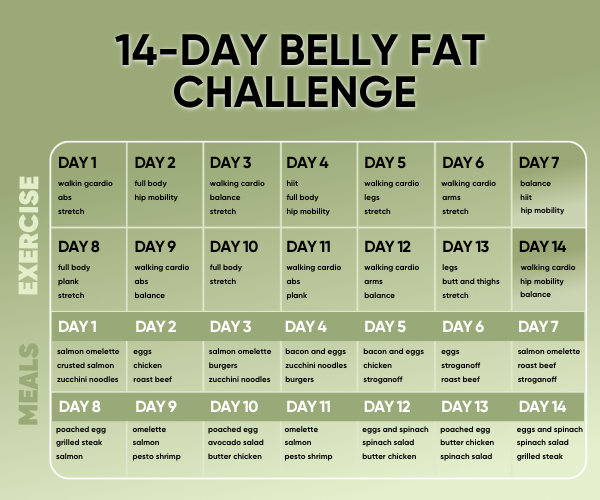
- Strength training 2–3 times a week to support bones, muscle and metabolism
- Walking or low-impact cardio most days for heart health and mood
- Protein, fibre and healthy fats (olive oil, nuts, seeds, oily fish) to steady blood sugar, support weight and reduce inflammation.
- Sleep routines: regular bedtime, cool dark room, limited screens before bed
- Stress care: breathing exercises, yoga, journaling, time in nature
These habits are hormone-supporting tools your future self will be grateful for.
HRT and Medical Options
Hormone therapy (HRT/MHT) means giving back some estrogen (and usually progesterone if you still have a uterus) to relieve symptoms and protect bones.
- According to The North American Menopause Society, hormone therapy is the most effective treatment for hot flashes and genitourinary symptoms of menopause and helps prevent bone loss.
- For most healthy women younger than 60 or within 10 years of menopause, the benefit–risk profile is considered favourable when there are bothersome symptoms.
It’s not right for everyone. Risks depend on:
- Type and dose
- How long you use it
- Personal and family history (e.g. breast cancer, clots, stroke)
This is a very individual decision, so always discuss it with your doctor or menopause specialist.
Supplements and Extra Support
Some women use:
- Calcium and vitamin D (bone health)
- Omega-3s (heart and brain support)
- Magnesium (sleep, muscle relaxation)
Evidence varies, and supplements can interact with medications, so it’s wise to discuss any new supplement with a healthcare professional.
READ ALSO: Top 10 Menopause Supplements for Women over 50
Key Hormone Facts You Can Keep in Mind
Quick reference to remember:
- Average age of menopause: around 51–52.
- Perimenopause can last: several years (often 4–8), but varies widely.
- Symptoms can last: some women have mild symptoms, others have moderate to severe symptoms for 7–10 years or more.
- HRT symptom relief: many women notice improvement in hot flashes and sleep within a few weeks; full benefit can take a few months.
Always contact a doctor promptly if you notice:
- New or severe chest pain
- Sudden shortness of breath
- Very heavy or unusual bleeding
- Sudden severe headaches or neurological symptoms
- Major mood changes, including thoughts of self-harm
A Simple 5-Step Plan to Support Your Hormones After 50
- Track symptoms for 2–4 weeks (sleep, mood, periods, hot flashes)
- Book a check-up (blood pressure, heart, basic bloods, discuss HRT if appropriate)
- Start strength and walking 3–5 days a week
- Shift food to “protein + plants first” (links to your bundle)
- Create a calm evening routine (lower lights, no caffeine, simple breathing)
Common Myths About Hormones in Menopause (and the Truth)

- “It’s all in your head.” No. Menopause involves real, measurable hormonal changes that affect the entire body and brain. Your symptoms are valid and biological.
- “Weight gain is inevitable and can’t be changed.” Weight gain is common but not hopeless. Adjusted nutrition, movement, strength training and sometimes medical support can make a big difference.
- “You can’t build muscle after 50.” You absolutely can. Studies consistently show women in midlife and beyond can gain muscle and strength with proper resistance training and protein intake.
- “HRT is always dangerous for everyone.” Not true. Modern guidance shows that, for most healthy women under 60 or within 10 years of menopause, benefits often outweigh risks. It still must be individualized.
When Should I Talk to My Doctor About Hormone Changes?
When your hormones are shifting, it can be hard to know what’s “normal menopause” and what needs urgent attention but some symptoms should always be checked by a doctor, just to be safe.
If something feels sudden, intense, or very different for you, it’s important not to ignore it or wait it out on your own.
Red flag symptoms to never ignore
- Very heavy bleeding, or any bleeding that starts again after 12 months without a period
- Chest pain, shortness of breath, or sudden severe headaches
- Thoughts of harming yourself, very low mood, or severe anxiety you can’t shake
- Sudden vision changes, strong heart palpitations, or any unusual or severe pain
Closing Thoughts
Menopause is a normal part of a woman’s life that all women experience. Although the hormonal changes that occur during menopause can be difficult, there are many things you can do to help keep hormones in balance and relieve symptoms.
If you understand the role of estrogen in menopause, the hormonal changes that happen, and the different ways to support hormonal balance, you can take charge of your hormonal health and make smart decisions about your treatment options.
Whether you use natural remedies or go to the doctor, the most important thing is to accept that you are going through menopause and help your body through this natural stage of life.
Remember that menopause is not a sign of aging but rather a new stage of life with new opportunities for growth and self-discovery.
This article is educational only, always seek medical advice for anything worrying or new.
Frequently Asked Questions About Hormones in Menopause
Many menopause symptoms are common, such as hot flashes, night sweats, brain fog, mood swings, irregular periods, and sleep problems, but anything that is sudden, severe, or feels very “not you” should be checked by a doctor. Very heavy bleeding, bleeding that starts again after 12 months without a period, chest pain, shortness of breath, sudden severe headaches, new vision changes, strong heart palpitations, or thoughts of harming yourself are not something to “wait and see” about and need urgent medical advice. This article is educational only – always speak to a health professional if you’re unsure or worried.
During perimenopause, estrogen doesn’t just slowly drop, it swings up and down, which is why symptoms can feel so unpredictable. Over time, your ovaries make less and less estrogen, your periods eventually stop, and in postmenopause your estrogen settles at a much lower, more stable level than before. This lower estrogen affects many parts of your body such as bones, brain, heart, skin, and weight, which is why so many different symptoms can show up at the same time.
Blood tests can sometimes show hormone changes such as a high FSH level, but they don’t always give a clear yes-or-no answer, especially in perimenopause when levels fluctuate a lot. For many women over 45, doctors often diagnose perimenopause or menopause based mainly on symptoms and changes in periods, rather than relying only on blood tests. If you’re younger, have irregular cycles, or symptoms that don’t fit the usual pattern, your doctor may order blood tests to help rule out other causes and decide on the best treatment.
You don’t have to take HRT; it’s one option, not the only option. Some women feel much better with lifestyle changes, non-hormonal medicines, or other treatments, while others find HRT gives them significant relief from symptoms like hot flashes, sleep problems, mood changes, and vaginal dryness. The “right” choice depends on your symptoms, medical history, personal preferences, and your doctor’s advice, so it’s about finding a plan that feels safe and sustainable for you, whether that includes HRT or not.
Menopause is not just the last period, it’s a longer hormone transition, and symptoms can continue for several years after your periods have completely stopped. Your body and brain are adjusting to a new, lower level of estrogen and progesterone, and this ongoing shift can still affect your temperature control, sleep, mood, joints, skin, and energy. The good news is that symptoms often change over time, and many women find that the right mix of lifestyle support, medical care, and self-care makes this stage much more manageable.
Yes, hormone changes in perimenopause and menopause can play a big role in low mood, irritability, tearfulness, anxiety, and feeling “not like yourself,” even if nothing else in your life has changed. Fluctuating estrogen and progesterone can affect brain chemicals linked to mood, stress, and sleep, which is why some women notice new or worse depression or anxiety around this time. That said, serious or ongoing mood symptoms still deserve proper mental health support, and it’s important to talk to a doctor or therapist if you’re struggling, especially if you ever feel hopeless or have thoughts of harming yourself.
For most women, the wild ups and downs of perimenopause eventually settle once you’re in postmenopause, when estrogen and progesterone levels stay low but more stable. Some symptoms naturally ease with time, while others such as, vaginal dryness or bone loss risk, may continue and need ongoing care. Every woman’s experience is different, but with the right support, many women find a new “steady state” where they understand their bodies better and feel more in control again.
This article was first published in May 2023 and last updated on November 26, 2025.